Walden University Pre-Written Nursing Academic Papers
Comprehensive Collection of Nursing Papers
You can learn about our extensive selection of Walden University Online BSN pre-written academic papers related to nursing. We offer a variety of resources, including case studies, research articles, care plans, and reflective essays that align with APA guidelines. Each paper covers relevant topics, providing essential insights for nursing students.
Custom Paper Assistance
For students seeking tailored support, our custom paper assistance allows them to submit requests based on specific assignment needs. It’s important to note that these papers are intended for reference purposes only and are intended to guide students toward successful academic outcomes.
Templates and Examples for Nursing Papers
In addition to pre-written papers, we provide templates for various nursing assignments, such as PICOT questions and nursing theories. Students can easily modify these examples to fit their requirements, making writing more accessible and efficient.
Description
SAMPLE PAPER
Walden University
Week 2 Assignment 1
To prepare:
- Reflect on your experience as an advanced practice nurse and on the information provided in the Week 1 Learning Resources on building a health history and the Week 2 Learning Resources on diversity issues in health assessments.
- By Day 1 of this week, your Instructor will assign a case study for this Assignment. Note: Please see the Course Announcements section of the classroom for your Case Study Assignment.
- Reflect on the specific socioeconomic, spiritual, lifestyle, and other cultural factors related to the health of your assigned patient.
- Consider how you would build a health history for the patient. What questions would you ask? How might you target your questions based on the patient’s social determinants of health? How would you frame the questions to be sensitive to the patient’s background, lifestyle, and culture?
- Identify any potential health-related risks, based on the patient’s age, gender, ethnicity, or environmental setting, which should be taken into consideration.
- What risk assessment instruments would be appropriate to use with this patient?
- What questions would you ask to assess the patient’s health risks?
- Select one (1) risk assessment instrument discussed in the Learning Resources, or another tool with which you are familiar, related to your selected patient.
- Develop five (5) targeted questions you would ask the patient to build their health history and to assess their health risks.
- Think about the challenges associated with communicating with patients from a variety of specific populations. What communication techniques would be most appropriate to use with this patient? What strategies can you as an APRN employ to be sensitive to different cultural factors while gathering the pertinent information?
Assignment: Building a Health History With Cultural and Diversity Awareness
Include the following:
- Explain the specific socioeconomic, spiritual, lifestyle, and other cultural factors associated with the patient you were assigned. Be specific.
- Explain the issues that you would need to be sensitive to when interacting with the patient, and why.
- Describe the communication techniques you would use with this patient. Include strategies to demonstrate sensitivity with this patient. Be specific and explain why you would use these techniques.
- Summarize the health history interview you would conduct with this patient. Provide at least five (5)targeted questions you would ask the patient to build their health history and to assess their health risks. Explain your reasoning for each question and how you frame each for this specific patient.
- Identify the risk assessment instrument you selected, and then justify why it would be applicable to your assigned patient. Be specific.
BY DAY 7 OF WEEK 2
Submit your Assignment.
SUBMISSION INFORMATION
Before submitting your final assignment, you can check your draft for authenticity. To check your draft, access the Turnitin Drafts from the Start Here area.
- To submit your completed assignment, save your Assignment as WK2Assgn1_LastName_FirstInitial
- Then, click on Start Assignment near the top of the page.
- Next, click on Upload File and select Submit Assignment for review.
SAMPLE PAPER
Week 2 Assignment 1
Student Name
Walden University
NURS – 6512C
Instructor’s Name
Date
Week 2 Assignment 1
Case Study
When constructing a health history for WH, a 62-year-old Chinese male with limited English, how several sociocultural, religious, and lifestyle factors affect his healthcare experience should be taken into consideration. The socioeconomic status of WH and potentially relying on his daughter to help him with caregiving as well as translating could greatly affect his healthcare access and ability to follow through with his schedule. Linguistic barriers may arise due to his poor English comprehension, making it difficult for him to follow medical advice, such as following his newly prescribed anti-hypertensive medication. However, spiritual beliefs could also play a role in determining WDH’s choice of treatment since WH might be a widower and could uphold the traditional Chinese cultural norms, which might prefer Traditional Chinese Medicine (TCM). His diet habits could also come into play as part of the factors influencing his hypertension, especially if he consumes foods rich in sodium out of the numerous traditional Chinese foods available. These cultural factors, combined with the possibility of developing thoughts of being a burden to his family, must be considered when evaluating his mental and physical health (Matos et al., 2021).
When dealing with WH, such matters should be delicately addressed. Due to linguistic differences, there are communication challenges, and they require the use of a qualified medical interpreter. As much as he might use his daughter to interpret for him, there could be cases where they do not understand each other or even feel uneasy when it comes to issues to do with health. However, it is also imperative that WH understands and remarks on the cultural beliefs and practices of other individuals. For example, he may not go for treatment or adhere to a prescribed treatment regimen because of cultural beliefs that lack facilitating resources and do not wish to burden his kin. Understanding these cultural characteristics is valuable in carrying out the rapport to improve trust with WH and improve the extent of his disclosure about any health issues.
Lack of interpersonal communication skills is another factor of importance in this regard. The choice of a professional interpreter guarantees that WH comprehensively comprehends the information that was shared with him and that he feels at ease talking about his health concerns without putting his daughter on the receiving end. Some of the things that may be helpful in communication are non-judgmental and culturally appropriate language, the lack of medical terminologies, and long, complex sentences that may be difficult for WH to understand (Liu et al., 2022). Using open questions may help WH to reveal more information on his concerns, ideas, and experiences based on his health, which could be beneficial for further care. Asking questions, paraphrasing, and summarizing are also important for building rapport and trust, as they involve expressing understanding of WH’s thoughts and emotions. Also, it is important to avoid eye contact, which makes overstorey WH uncomfortable, and gestures that are not acceptable in their respective cultures (Su et al., 2020).
Specifically, in the course of obtaining a health history interview, I would avoid general questions and instead ask questions that are specific, culturally appropriate, and considerate of WH. For instance, ascertaining whether he has used natural or traditional medicines or treatments reveals the possible TCMs that may pose interference with the prescribed drugs. It is appropriate to ask the man about his native customs and traditions without offending him or dwarfing his culture. Another essential question would be to ask WH if he has feelings about the new medication that was prescribed to him and whether he has noticed any difference since he began taking it. This enables WH to report to the doctor any discomfort he may be experiencing as a result of the medication or other side effects, which are important for him to adhere to the prescribed plan (Wang et al., 2021). Furthermore, I would question him about his diet and exercise regimen because these concerns fall under the category of hypertension management. It is also crucial to consider his mental health and his emotional response since the death of his wife to overall care for him.
In evaluating WH’s cardiovascular risk, I would apply the Framingham Risk Score, which calculates the individual’s 10-year cardiovascular risk based on his or her age, cholesterol levels, blood pressure, smoking status, and diabetes. This tool is applicable in WH’s case, given his age and hypertension, since it offers a holistic report of his cardiovascular health. With this particular instrument, I am able to focus on particular risk factors that may need to be addressed in order to enhance his health profile.
Lastly, developing a health history for WH requires more than merely collecting his medical background, but also acknowledging the cultural, socio-economic, and spirituality roles that touch his health. When using suitable communication that is sensitive to culturally appropriate care and choosing the right assessment tools, it will be possible to give WH quality care that was founded on his culture.
References
Matos, L. C., Machado, J. P., Monteiro, F. J., & Greten, H. J. (2021, March). Understanding traditional Chinese medicine therapeutics: an overview of the basics and clinical applications. In Healthcare (Vol. 9, No. 3, p. 257). MDPI.
Liu, Y., Li, B. G., Su, Y. H., Zhao, R. X., Song, P., Li, H., … & Ren, X. (2022). Potential activity of traditional Chinese medicine against ulcerative colitis: a review. Journal of ethnopharmacology, 289, 115084.
Su, X. L., Wang, J. W., Che, H., Wang, C. F., Jiang, H., Lei, X., … & Wang, Q. H. (2020). Clinical application and mechanism of traditional Chinese medicine in treatment of lung cancer. Chinese Medical Journal, 133(24), 2987-2997.
Wang, W. Y., Zhou, H., Wang, Y. F., Sang, B. S., & Liu, L. (2021). Current policies and measures on the development of traditional Chinese medicine in China. Pharmacological research, 163, 105187.
Week 3 Assignment 1
To prepare:
- By Day 1 of this week, your Instructor will assign a patient profile for this Assignment. Note: Please see the Course Announcements section of the classroom for your patient profile Assignment.
- Review this week’s Learning Resources.
- Review the details of the patient case study.
- Consider what physical exams and diagnostic tests would be most appropriate to gather more information about the patient’s condition.
- Reflect on how the results would be used to make a diagnosis.
- Identify three to five (3–5) possible conditions that may be considered in a differential diagnosis for the patient.
Assignment: Diagnostic Reasoning
Include the following:
- Identify the patient’s chief complaint.
- Identify what physical exams and diagnostic tests would be most appropriate to gather more information about the patient’s condition. Be specific and explain your reasoning.
- Explain how the results would be used to make a diagnosis.
- Identify three to five (3–5) possible conditions that may be considered in a differential diagnosis for the patient. Explain your thinking.
BY DAY 7 OF WEEK 3
Submit your Assignment.
SUBMISSION INFORMATION
Before submitting your final assignment, you can check your draft for authenticity. To check your draft, access the Turnitin Drafts from the Start Here area.
- To submit your completed assignment, save your Assignment as WK3Assgn1_LastName_FirstInitial
- Then, click on Start Assignment near the top of the page.
- Next, click on Upload File and select Submit Assignment for review.
SAMPLE PAPER
Week 3 Assignment 1
Student Name
Walden University
NURS – 6512C
Instructor’s Name
Date
Case Study: Miss Washington
Chief Complaint
The patient is a 71-year-old female, Miss Washington, who has presented with a new leg ulcer that developed after she fell last week. She also presents with complaints of coughing, wheezing, and feeling ill, “I’m feeling terrible.” However, her vitals are normal, and she has no fever. The main concern regarding this patient is the presence of the leg ulcer and respiratory signs (coughing and wheezing); the patient complains of being very uncomfortable.
Physical Exams and Diagnostic Tests
Several physical examinations and diagnostic tests are required to get more information on the case of Miss Washington. First, a complete physical check-up should be done. This involves a global appreciation of her physical state and the first observations with a special emphasis on sniffing for signs of discomfort, pallor, or cyanosis. As for vital signs, there is no serious pathology; however, assessing her overall condition may reveal other signs of a systemic process. The assessment of the respiratory system highlights wheezing, crackles, and loss of breath sounds suggestive of pneumonia, COPD, or asthma, particularly in immunocompromised patients (Pal et al., 2020). Moreover, vital signs such as the respiratory rate and oxygen saturation should be assessed to evaluate the condition of the respiratory system.
Because of her age and various presented respiratory signs, it is also necessary to perform a cardiovascular examination. This involves auscultation of the heart to check for heart failure or cardiovascular disease that might have a role in the respiratory diseases that affect her. The fact that a leg ulcer is present indicates the need for further discussion. The ulcer must be assessed for size, depth, color, and presence of infection indicators such as redness, warmth, or pus-like discharge. In nursing assessment, a light touch on the ulcer and its surrounding area can be done to determine whether the area is tender, warm, or poorly perfused, and the pulses in the affected limb should be checked. Furthermore, an ankle-brachial index test will also help determine the presence of arterial disease, which may hinder the wound healing process. A neurological assessment may also be required to exclude any possibility of neurological injury from the fall.
Regarding diagnostic tests, wound culture is critical in order to decide if the leg ulcer is infected and, if infected, to identify the causative microorganisms and, thus, the correct antibiotic treatment. A complete blood count (CBC) is required to check for signs of infection and possible anemia. A high white blood cell count suggests she may have an infection; low hemoglobin might explain why she feels unwell and could slow the healing of wounds (Seo & Lee, 2022). A BMP is also ordered to check the electrolytes and renal function, which could suggest a systemic cause of her weakness. Considering the respiratory signs, a chest x-ray is mandatory to exclude pneumonia, COPD flare-up, or any other pulmonary process. Last, a Doppler ultrasound of her leg should be performed to rule out DVT, which may be a cause of the leg ulcer and is more likely after trauma. A venous or arterial duplex ultrasound should then accompany this to identify any blood flow problems and vascular insufficiency.
How the Results Can be Used for Diagnosis
The outcome of these tests will assist Miss Washington’s physicians in determining which treatment plan is best for her. A wound culture will indicate whether there is a bacterial infection on the ulcer, directing the right antibiotic treatment. If CBC revealed high white blood cells, then this would imply there was an infection, which may have caused all the general body symptoms she was exhibiting. If anemia is present, this may point to her general weakness and slow wound healing. She should undergo BMP, which will give information about her electrolyte levels and renal functions and exclude systemic causes of her symptoms, such as dehydration or renal disease.
An X-ray of her chest will be essential in checking whether she has respiratory issues that may include pneumonia or a flare-up of COPD that may cause her to have a cough and wheeze. Abnormalities like infiltrates for pulmonary causes would require antibiotics for treating pneumonia, while hyperinflation or other features might suggest an exacerbation of COPD. A positive Doppler ultrasound for DVT would warrant anticoagulation therapy, which could have contributed to her respiratory symptoms, such as a pulmonary embolism.
Differential Diagnosis
The case of Miss Washington lists several plausible diseases that may have led to her symptoms. This may include venous ulcer, which is common in elderly patients, particularly with a history of injury to the affected limb. The worsened status of the patient’s leg ulcer could be due to either poor venous return or delayed healing. She coughs and wheezes; it may just be that the patient had a slight respiratory tract infection. In this case, there are other potential reasons, including cellulitis with a secondary bacterial infection. The leg ulcer may be infected, and a patient may present with other signs that suggest he or she is unwell (Hess, 2020). Therefore, the infection cannot be discounted even when the patient is afebrile, more so if the individual is elderly, because the clinical picture may not be an acute febrile response that is familiar in an infective process.
Congestive heart failure should also be excluded, as she also has a cough, and a history of wheezing may indicate a COPD flare. This disease is prevalent in patients with other diseases, especially in elderly patients; there may be a worsening of the disease due to infection or changes in the environment (Grassi et al., 2021). The respiratory complications, which may include coughing, wheezing, or shortness of breath, present in this disorder could be due to lung diseases like cystic fibrosis or emphysema if she smokes or has asthma. Another disorder is congestive heart failure (CHF), as congestion of the lungs leads to cough, wheezing, and fatigue associated with CHF. Her leg ulcer may take time to heal because there is inadequate blood supply to the lower limbs, as seen in heart failure patients.
Last but not least, a diagnosis of pulmonary embolism (PE) should be considered, more so since she fell a few days before coming to the hospital and the possibility of DVT. Depending on the severity and type of PE, a patient with a PE might not show pulmonary signs such as coughing and wheezing or experience marked hypoxemia, provided it is microembolism (Freund et al.., 2022). Due to the presence of a leg ulcer and she is above 60 years of age, she is at a higher risk of developing DVT, and without treatment, a PE may occur.
Conclusion
In a way, Miss Washington’s presentation demands coordinated diagnostics where physical examination, the state of the wound, respiratory condition, and vascular studies all enter the differential equation. The tests mentioned will assist in ruling out which of the possible diagnoses is likely to be causing her leg ulcer, cough, and wheezing. The potential differential diagnoses of venous ulcer, cellulitis, COPD exacerbation worsened CHF, and pulmonary embolism demonstrates the complexity of her case, and further investigation will aid in defining her treatment plan.
References
Grassi, G., Quarti-Trevano, F., & Esler, M. D. (2021). Sympathetic activation in congestive heart failure: an updated overview. Heart Failure Reviews, 26(1), 173-182.
Freund, Y., Cohen-Aubart, F., & Bloom, B. (2022). Acute pulmonary embolism: a review. Jama, 328(13), 1336-1345.
Hess, C. T. (2020). Venous ulcer assessment and management: using the updated CEAP Classification System. Advances in skin & wound care, 33(11), 614-615.
Pal, M., Berhanu, G., Desalegn, C., & Kandi, V. (2020). Severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2): an update. Cureus, 12(3).
Seo, I. H., & Lee, Y. J. (2022). Usefulness of complete blood count (CBC) to assess cardiovascular and metabolic diseases in clinical settings: a comprehensive literature review. Biomedicines, 10(11), 2697.
Week 3 Assignment 2
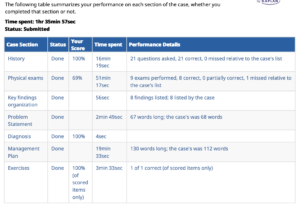
I-HUMAN PRACTICE CASE
As part of your orientation to i-Human Patients, you are required to explore the Marvin Webster, Jr. practice case to become familiar with the i-Human Patients interface and to start making the transition between the live patient encounter and the virtual patient encounter.
Note: You are allowed five (5) attempts at this i-Human Patients Assignment. Your final submission is due by Day 7 of this week.
Also Note: The instructions for this practice case Assignment are repeated from Week 2 for your convenience.
To prepare:
- Be sure that you have thoroughly reviewed the i-Human Patients Case Player Student Manual in the Week 2 Learning Resources.
- Access the required i-Human Patients Marvin Webster, Jr. practice case study from the Week 2 Learning Resources.
Important Note: Once you have purchased your i-Human Patients access code from the bookstore, you should receive an email with your i-Human Patients login and password information. If you have not received this information, please contact the Course Instructor.
Assignment
As you interact with the Marvin Webster, Jr. i-Human Patients practice case, complete the assigned case study. Upload your PDF from i-Human Patients to this Assignment.
Note: There will be no additional attempts after your Final Assignment submission by Day 7.
BY DAY 7 OF WEEK 3
Submit your final attempt by uploading your PDF from i-Human Patients to this Assignment.
SUBMISSION INFORMATION
Before submitting your final assignment, you can check your draft for authenticity. To check your draft, access the Turnitin Drafts from the Start Here area.



Reviews
There are no reviews yet.